How Blood Sugar Affects Your Adrenals
Blog
How Blood Sugar Affects Your Adrenals
Ever been chased by a bear?
If so, your adrenal glands probably saved your life.
Your adrenal glands are the reason you can run away from an onrushing bear. They are the reason you’re able to get out of bed in the morning. They are the reason a mother can suddenly possess the strength to lift a car off her trapped child!
Your adrenals sit perched on top of your kidneys. These powerful little organs produce several hormones that are necessary for survival.
But unfortunately, many of us have asked too much of our adrenals. We have pushed them to the limit. They’re worn out, and they struggle to keep us chugging along.
What exactly do the adrenals do?
The adrenal glands play a vital role in the delicate dance of blood sugar regulation. When we flood our body with sugar, the pancreas releases insulin (a hormone) to help store away all that excess sugar. Often, the pancreas will overcompensate and release more insulin than is needed.
The result? Low blood sugar. This is why you experience a crash after a big, sugary treat.
Low blood sugar is very dangerous. It can cause weakness, dizziness, fainting, or death. The body views this as an emergency, and that’s where the adrenals come in. You adrenals will produce epinephrine, norepinephrine, and eventually cortisol to save the day.
Epinephrine & Norepinephrine
When your nervous system senses stress—in this case, low blood sugar—it will send a signal to the adrenals to prepare for a fight or flight.
The adrenals then release epinephrine and norepinephrine which increase your heart rate, dilate your pupils and lungs, and increase your blood sugar (NTA, 2019). Norepinephrine also raises your blood pressure.
Cortisol
Cortisol, another “stress hormone”, similarly frees up glucose (sugar) in the body in stressful situations.
The hypothalamus and pituitary (regions of the brain) are the conductors that tell the adrenals to release cortisol when blood sugar is too low.
Where the dysfunction happens
In the ideal situation, the adrenals would only play a subtle role in blood sugar regulation. You would eat a meal high in carbohydrates (carbohydrates turn into sugar in the body), blood sugar would rise, and the pancreas would release insulin to lower blood sugar.
Then, if necessary, the adrenals might fire up some hormones to help bring blood sugar back to an optimal level.
Unfortunately, because of the all-too-common Standard American Diet (SAD), this is seldom the reality. The Standard American Diet is one full of sugar. There’s added sugar everywhere: in our breakfasts, in our coffee, in our condiments, in our protein bars.
From the 18th to the 21st century, Americans went from eating an average of 4 pounds of sugar a year to about 180 pounds of sugar a year per person (United States Department of Agriculture, 2017). When we eat sugar all day long, we ask our adrenals to continually pump out epinephrine and cortisol with no break.
What’s worse, high blood sugar is not the only stressor on the adrenals. Our modern lifestyles, marked by busy days, low sleep, and environmental toxins, are also notoriously stressful.
Our brain sees this stress and signals to the adrenals to pump out even more cortisol to keep us going.
Eventually, this chronic stress can develop into something called HPA Axis Dysregulation. This is when the HPA Axis, which the Nutritional Therapy Association (2019) refers to as “a complex set of interactions between the hypothalamus, the pituitary gland, and the adrenal glands”, is not working as it should.
This can manifest itself in many different ways, including:
- Chronic fatigue
- Difficulty sleeping
- Memory problems
- Brain fog or difficulty concentrating
- Hormonal imbalances
- Reduced libido
- Skin problems
You may have heard the antiquated term for this, “adrenal fatigue”. It was replaced because it inaccurately implies the adrenals are the only organ involved.
Chronic stress affects the entire HPA axis (hypothalamus, pituitary, and adrenals), and the dysfunction may not be related to the adrenal’s ability to produce enough hormones.
The dysfunction might be coming from further up the chain (hypothalamus or pituitary).
Supporting your HPA Axis through blood sugar management
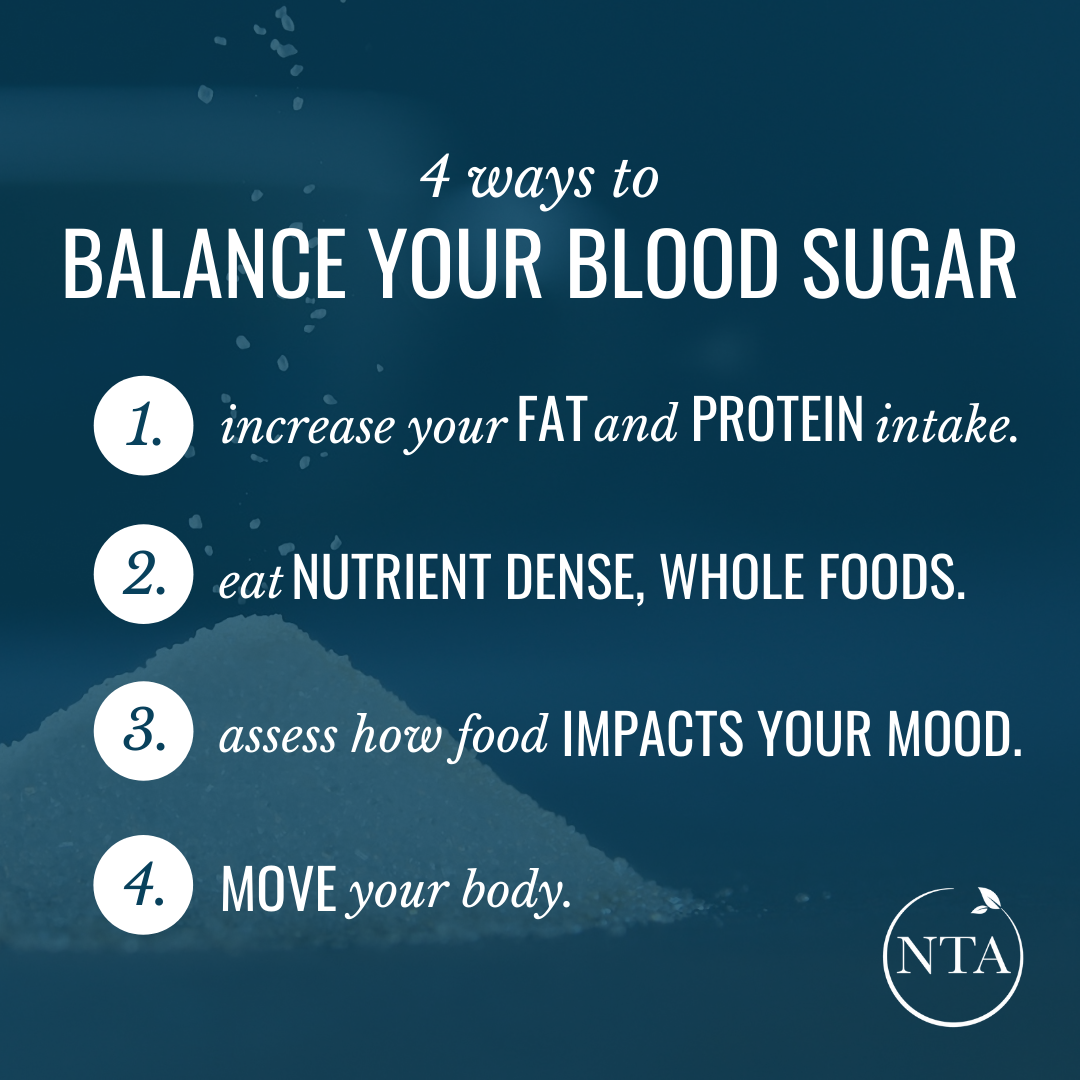
Keeping in mind that HPA Axis dysfunction is typically complicated and multifactorial, here are few things you can do to balance your blood sugar and thereby support your adrenals and the rest of your HPA Axis:
1. Increase your fat and protein intake
Increase the fats and protein in your diet to ensure your body is getting a balance of all three macronutrient fuel sources (fat, protein, and carbs).
Focusing on trying to cut out processed sugar and refined grains can be a mistake. Try focusing on what you can add into your diet that will support your body and help you feel great.
2. Eat nutrient-dense, whole foods
There are a variety of nutrients that support blood sugar regulation, including vitamin A, many of the B vitamins, chromium, potassium, etc. We get these from whole foods from the earth. Vegetables, meat, nuts, fruit, etc.
Look, we’re not looking for perfection here. However, what you’re fueling your body with most of the time can make a big impact on the way you feel.
3. Assess how food impacts your mood
Is food your go-to source of comfort? Do you feel guilt and shame if you eat a treat that sends you spiraling into a full-blown binge?
Maybe you don’t need to go on a 30-day low-sugar diet right now. Maybe you need to take a deeper look at the foods you are eating and why are you feeling this way.
4: Move your body
Walking, running, vacuuming, lifting, break-dancing, chasing your children around, hot yoga. Don’t worry too much about how you do it; what matters most is that you do it.
Movement helps you process out your stress hormones and use up that excess blood sugar.
Common, but not normal
Blood sugar wackiness that ruins your day and HPA Axis Dysfunction may be common, but they are not normal.
By focusing on a nutrient dense, whole food diet full of proteins, fats, and carbohydrates, we each have what it takes to help our bodies find restoration and balance.
This article was written by NTA grad, Ayla Freitas Ghibaudy
Ayla is a Nutritional Therapy Practitioner and advocate for body neutrality. She is the creator of Eating Sensibly, a nutrition resource hub that promotes self-care and self-advocacy, and the author of Body Neutrality. Her mission is to empower women to freely live out their calling, unencumbered by diet culture or negative body image.
You can find Ayla through her website, www.eatingsensibly.co and Instagram.
The views and opinions expressed in this post are those of the author and do not necessarily reflect the views and opinions of the NTA. They are intended for general information purposes, and are not to be considered a substitute for medical advice, diagnosis, or treatment. Want your recipe or article to be featured on our blog? Email our team Marketing@nutritionaltherapy.com with your full name, article, a short bio in third person, and a headshot. We may feature you in an upcoming blog post.
Resources:
- Nutritional Therapy Association (2019). Blood Sugar Regulation Module Study Guide. Olympia, WA.
- United States Department of Agriculture. (2017). Food Availability and Consumption. hlps://www.ers.usda.gov/data-products/ag-and-food-statistics-charting-the-essentials/food-availability-and-consumption

Join us for a Live Webinar with one of our Instructors and Admissions Advisors!
During this call, you’ll explore and learn:
- How to create a rewarding career in holistic nutrition that will give you the confidence and competence to replace your full-time income (whether you’re new to nutrition or or using it to enhance your current services)
- How our unmatched education and instructor support sets our NTP program apart from other nutrition programs
- How graduates are successfully using their education and the many career opportunities available to you
- If the NTP program is the right fit for you and how to move forward in financing your education


